January 12, 2024, 3:45 PM EDT
CDC is posting updates on respiratory viruses every week; for the latest information, please visit CDC Respiratory Virus Updates.
CDC Tracks Hospital Capacity as Respiratory Diseases Continue to Spread
This time of year, hospitals, including intensive care units, can get very busy because of people seeking care for respiratory symptoms. These additional demands on the healthcare system may make it hard for people to get medical care for both respiratory and non-respiratory conditions in a timely fashion. With COVID-19, flu, and respiratory syncytial virus (RSV) circulating at high levels and other respiratory illnesses occurring, it is possible that healthcare capacity may become strained in some places.
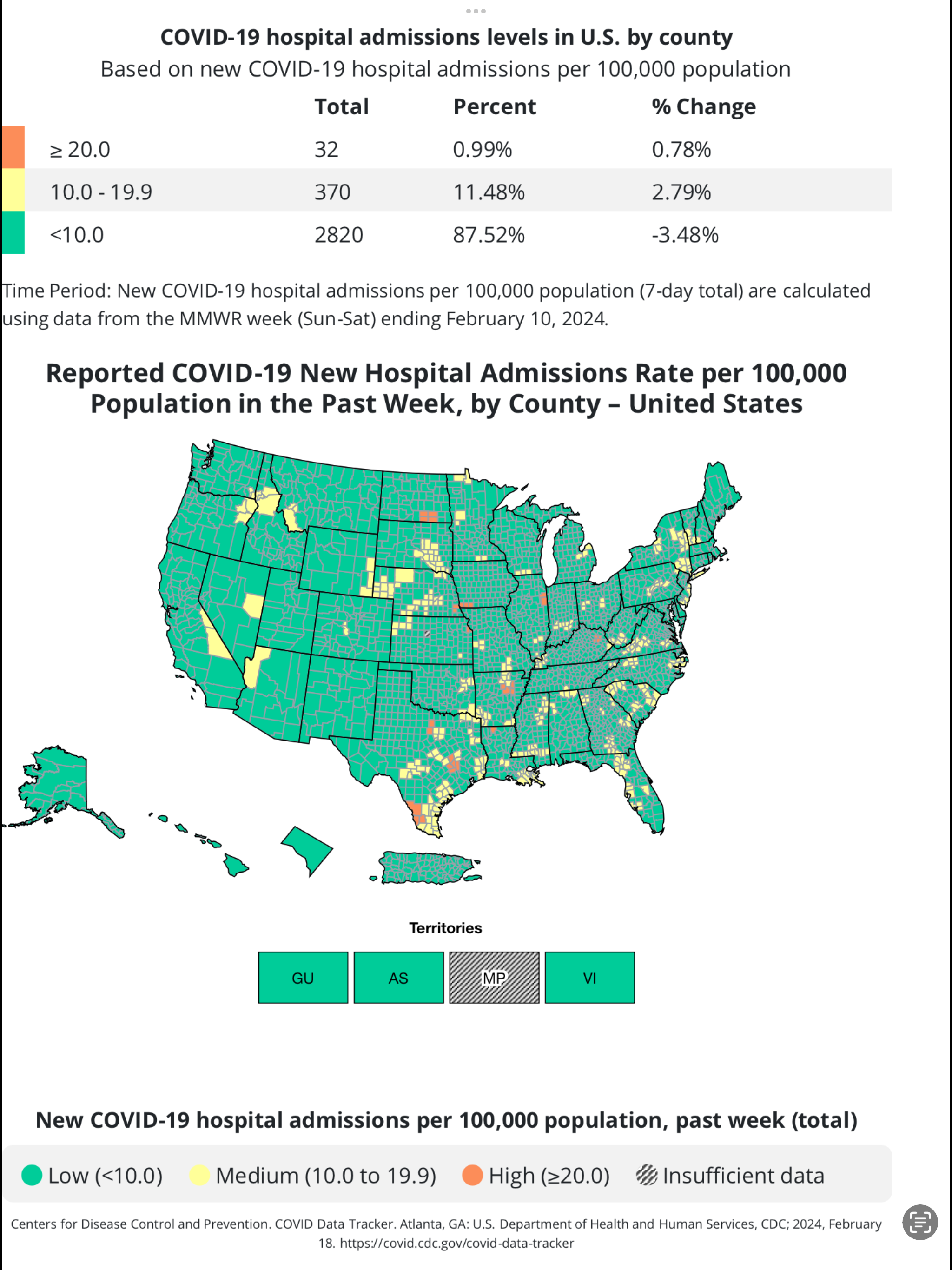
Hospital admissions for COVID-19, flu, and RSV remain elevated in many parts of the country and CDC is watching closely for signs of strain.
Strain on hospitals
Since the start of the respiratory virus season, overall hospital bed occupancy has been lower than last season in most of the United States. However, pediatric bed occupancy in some regions has been nearly as high or higher than last season. For instance, pediatric bed occupancy has been higher than last season in the Southeast, where respiratory disease activity has been elevated for longer.
On December 14, 2023, CDC put out a Health Alert Network health advisory warning that low vaccination uptake, coupled with rising levels of respiratory diseases, could lead to more disease and potentially more severe disease, straining healthcare capacity in the coming weeks. CDC continues to anticipate this respiratory disease season will likely result in a similar number of hospitalizations as last season, according to CDC’s most recent outlook.
In December, new hospital admissions for COVID-19 were up by more than 50%, while new hospital admissions for flu more than doubled from the end of November to the end of December. These increases are typical for this time of year, and short-term forecasts suggest elevated numbers of hospital admissions will continue.
CDC is closely monitoring the stress that respiratory illnesses is putting on the healthcare system. CDC shares these data with partners in federal, state, and local governments to inform healthcare planning and response. In addition to taking a toll on our healthcare workers, healthcare system strain has previously been associated with:
- delays in treatment and elective procedures,
- increased medical errors and lower quality of care,
- longer patient stays,
- increased rates of healthcare-associated infections, and
- poorer outcomes, including excess deaths.
COVID-19 has changed respiratory disease season
Prior to the COVID-19 pandemic, many hospitalizations due to respiratory illness were caused by flu and RSV. But COVID-19 changed respiratory illness patterns. During the 2020-2021 and 2021-2022 seasons, flu and RSV activity were significantly lower than usual.
The 2022-2023 season marked a departure from the previous two seasons, with flu and RSV circulating simultaneously with COVID-19 at high levels and peaking early. Pediatric hospital beds were in short supply, primary care offices were very busy, and demand for over-the-counter medications was higher than expected, leading to shortages in some areas.
The current season is the second season during which these three respiratory viruses have spread at high levels simultaneously. COVID-19 continues to cause a larger number of hospitalizations and has been involved in many more deaths than flu and RSV combined.
Tracking hospital capacity indicators
Although not perfect, hospitalization data are the best available data for monitoring healthcare capacity and strain. CDC tracks these data mainly through the National Healthcare Safety Network (NHSN), which collects COVID-19 and flu hospitalization and bed occupancy data from all hospitals nationwide. Also, the Respiratory Virus Hospitalization Surveillance Network (RESP-NET) provides data on COVID-19, flu, and RSV hospitalizations from sites across the country, covering about 10% of the U.S. population. CDC uses these data to track hospitalization trends for these three key respiratory viruses and signals of potential healthcare strain.
The NHSN data are collected weekly from all hospitals and made publicly available on CDC’s COVID Data Tracker. As rich as these data are, they don’t paint a full picture of hospital capacity; hospitals often manage their capacity by canceling elective procedures or using other mechanisms to free up hospital beds.
CDC supplements the NHSN information by communicating regularly with health departments across the country, as well as other public health and clinical partners. CDC also works closely with the Administration for Strategic Preparedness and Response (ASPR), another agency in the Department of Health and Human Services, to evaluate and respond to signals of healthcare strain. ASPR has regional representatives who work directly with healthcare systems experiencing strain to explore local, regional, and national options to address concerns.
What’s next?
Many people across the country are preparing in the event that some hospitals are strained because of a potential simultaneous peak of hospital admissions from COVID-19 and flu. CDC and ASPR are working with partners to minimize impact on healthcare delivery.
As a reminder, there are effective vaccines and antiviral treatments for COVID-19 and flu and immunizations for RSV, along with other simple ways to protect yourself and loved ones from COVID-19, flu, and RSV. By taking these steps, we can each play our part in reducing the burden on the healthcare system and workforce.
Original Article – https://www.cdc.gov/respiratory-viruses/whats-new/track-hospital-capacity.html