What is myocarditis?
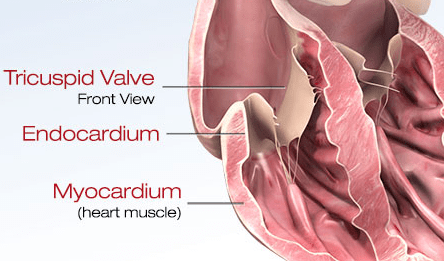
Myocarditis is a serious though rare condition where inflammation develops in the myocardium, or middle muscular layer of the heart wall.
Myocarditis can weaken the heart and its electrical system. As a result, the heart’s ability to pump blood declines.
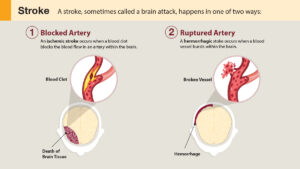
The condition may be acute and resolve quickly. Or it may be chronic, lasting longer than two weeks. In severe cases, myocarditis may lead to stroke, heart attack, heart failure or death.
Often the cause of myocarditis is unknown. Commonly a viral infection (such as a cold or flu), bacterial infection (such as diphtheria or strep), or fungal infection (such as candidiasis) can lead to myocarditis. Medications, autoimmune disorders, and toxic substances also can cause it.
What are the symptoms of myocarditis?
People with myocarditis don’t always have symptoms. Others have mild or severe signs, such as:
- Fatigue
- Shortness of breath
- Fever
- Chest pain
- Hard, rapid, or irregular heartbeat
- Light-headedness or fainting
- Flulike symptoms including headache, body ache, joint pain or sore throat
Some cases of myocarditis can feel like a heart attack. Seek emergency medical help immediately for unexplained chest pain or shortness of breath.
How is myocarditis diagnosed and treated?
A health care professional is needed to diagnose myocarditis. Patients will often get a physical exam and share their medical and family history. In addition, other procedures are used to diagnose the condition, including:
- Blood tests
- MRI (magnetic resonance imaging)
- Chest X-ray
- EKG/ECG (electrocardiogram)
- Echocardiograph
- Cardiac catheterization and biopsy
Myocarditis treatment targets symptoms and the underlying cause if it’s known. Those with mild myocarditis may only need rest and medication. Patients with severe cases may need lifelong medication, implanted devices or other surgeries.
Staying healthy
Proper heart function can be supported by lifestyle changes. Some of these include reducing sodium intake, avoiding alcohol, and quitting smoking. Patients with myocarditis are often advised to avoid competitive sports while active inflammation is present.
Myocarditis and COVID-19
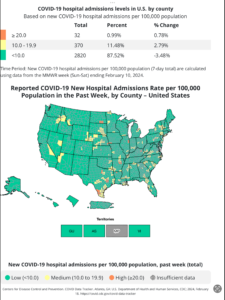
Health organizations such as the Centers for Disease Control and Prevention (CDC) continue to monitor whether myocarditis is linked to COVID-19. Researchers have published several studies on myocarditis and COVID-19 cases and vaccines since the start of the pandemic. Some include:
- An international study published in April 2022 found about 3 in every 1,000 patients hospitalized due to a COVID-19 infection developed acute myocarditis. The study used data from the first 15 months of the pandemic, before COVID-19 vaccines were widely available. Among those hospitalized for COVID-19 and diagnosed with myocarditis, those who also developed pneumonia were more likely to need a ventilator to breathe and had an increased risk of death.
- A December 2021 study found that most adolescents and young adults with suspected myocarditis following a COVID-19 vaccination have mild symptoms and rapid recovery. But the study notes that information on longer-term outcomes is lacking and future studies are needed.
- Myocarditis was reported at a higher rate than expected among some people who received the Pfizer or Moderna vaccines, according to a July 2021 study. Most of the suspected myocarditis cases in that study developed after the second dose and were among males between 12 and 39 years old. Despite these cases, the study stated that the benefits of the COVID-19 vaccine outweigh the rare risk of myocarditis.
Written by American Heart Association editorial staff and reviewed by science and medicine advisors. See our editorial policies and staff.
Last Reviewed: Sep 27, 2022
Original Article – https://www.heart.org/en/health-topics/myocarditis